The COVID-19 pandemic is an unprecedented challenge. The U.S. hasn’t suffered from a pandemic like this in more than a century. But other countries have recently had to deal with very frightening disease outbreaks, like the Ebola crisis in West Africa.
Nurses were squarely in the public eye: examined, criticized, and, at times, praised as singular heroes amidst failing institutions. The nation learned that some hospitals and regions are better prepared than others to address infectious disease epidemics; that nurses are on the front lines of care; and that, without adequate training and protection, nurses put their own health and safety in jeopardy to care for the public.
Ebola taught us painful but valuable lessons. Today, as our healthcare workers across the world confront COVID-19, we share those lessons and recommendations to strengthen the response.
What was the nurse’s responsibility in caring for a patient with Ebola?
- The nurses, in all professional relationships, had to practice with compassion and respect for the inherent dignity, worth, and uniqueness of every individual, unrestricted by considerations of social or economic status, personal attributes, or the nature of health problems.
- Nurses had to advocate, promote, and strive to protect the health, safety, and rights of the patient.
- Nurses had to owe the same duties to self as to others, including the responsibility to preserve integrity and safety, to maintain competence, and to continue personal and professional growth.
What were the specialized roles involved in identifying and controlling Ebola?
- Nurses played a key role in the direct care of patients with Ebola or other infectious conditions including assessing the patient, monitoring response to treatment, and assisting with activities of daily living.
- Physicians directed diagnosis and treatment of Ebola cases – infectious disease physicians and other specialists directed the medical treatment of patients.
- Public health officials were involved in case identification, contact tracing, and epidemiologic investigation.
- Emergency room nurses and intensive care nurses provided direct care of affected patients.
Listen to the below audio to know “what an ER nurse learned from Ebola outbreak and now COVID-19”
Why healthcare workers should take proper care of themselves?
Ebola killed nearly 1 out of 10 of Liberia’s healthcare workers. In the Lombardy region of Italy, the infection rate is 12% for health workers, versus 1% for the general population. Contracting the illness doesn’t only lower the number of workers available to fight the virus, it shatters the spirits of those left on the frontlines. Health workers, 70% of whom are women, get sick when they lack protective equipment. A nurse without protective equipment is like a soldier without a helmet – neither stands a chance against their enemy.
What are isolation precautions and why are they used?
- Isolation precautions are a set of interventions used to prevent the spread of infectious diseases. These include standard precautions (applied to all patients) and transmission-based precautions (recommended based on the way that an infection is transmitted).
- Enhanced isolation is recommended for specific infections. The recommendation to cover all exposed skin and supervise donning and doffing of PPE is an example of enhancements to isolation.
What is Personal Protective Equipment (PPE)?
- PPE includes gowns, gloves, masks, boots.
- Along with PPE, hand hygiene and environmental controls are important parts of isolation precautions.
Why is PPE worn?
- The use of PPE is required according to the nurse practice acts.
- PPE is used to:
- Protect healthcare workers.
- Protect patients from cross-transmission.
- Prevent environmental contamination.
Where can current evidence-based practice guidelines be found?
Current practice guidelines for different settings are available from:
- International bodies (WHO)
- National agencies (CDC)
- Professional associations (APIC, SHEA, IDSA, ANA, NLN)
- Hospitals and other healthcare facilities develop guidelines, policies, and procedures for the care of patients with highly contagious conditions.
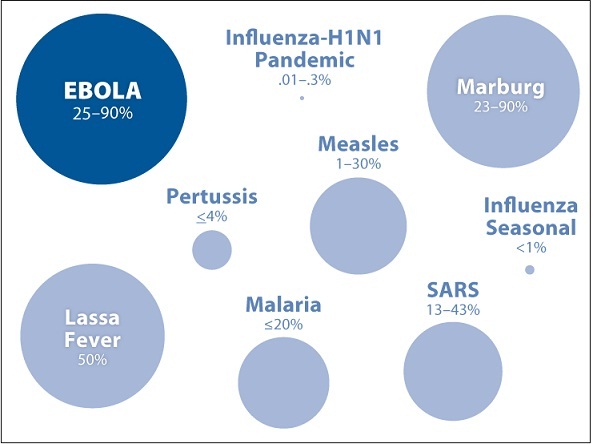
How deadly was Ebola?
What is the final message?
When epidemics strike, fear, anxiety, and despair can be agonizing. But as we learned during the Ebola epidemic, we are not defined by the conditions we face, no matter how hopeless they seem – we are defined by how we respond to them. Decisive political leadership and global cooperation – along with every single one of us playing our part – will determine if we win the war against this invisible enemy.
“The difference between who you are and who you want to be is what you do.”