About the novel coronavirus (COVID-19) outbreak
Since December 2019, multiple clusters of COVID-19 cases have been reported across more than 70 countries which include highly affected Italy, Iran, Japan, South Korea, and the United States.
The U.S. Department of Health and Human Services declared the virus to be a nationwide health emergency following the World Health Organization’s (WHO) declaration of a public health emergency of international concern on January 30, 2020.
The first death due to COVID-19 in the United States was reported in Kirkland, Washington State, on February 29, 2020. Since then, the number of new cases and deaths and been accelerating exponentially. The timeline of the virus has been accelerating at a frightening rate. But just how big of a threat is coronavirus? Here’s what you need to know.
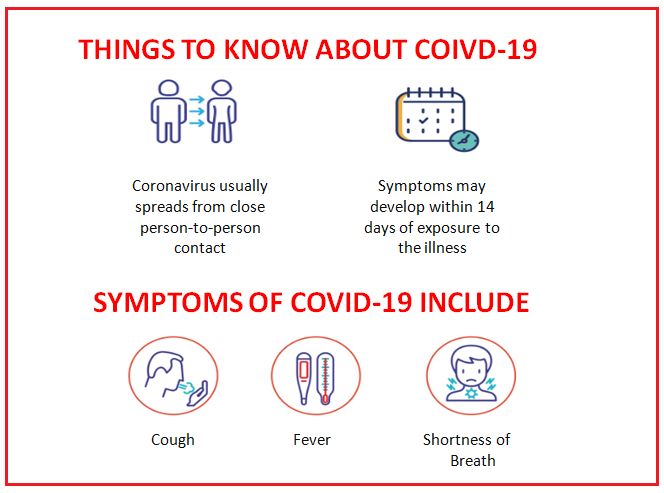
Coronavirus symptoms – as we all know
So far, the CDC says that 2019-nCoV or COVID-19 causes “mild to severe respiratory symptoms” (thanks, CDC, that’s a super helpful range) which have included:
- Fever
- Cough
- Shortness of breath
It’s thought that after exposure to the virus, one could develop symptoms in as few as two days, or as long as two weeks. The virus can prove fatal when it leads to other complications and lead to other organ shut down, such as pneumonia and kidney failure, etc.
How nurses are being affected?
The International Council of Nurses (ICN), along with the World Health Organization (WHO), has turned its focus onto the enormous toll that the virus is having on nurses caring for patients in affected areas.
In the coming weeks, the WHO plans to issue guidance in supporting the mental health of the staff caring for people affected by the virus. “Many nurses will be working long stressful shifts during which they are exposed to a great deal of human suffering,” the ICN explained in a statement. “Their mental wellbeing is extremely important if they are to be able to continue to provide the highest quality care possible.”
It’s hard to fathom what the nurses caring for infected patients—as well as patients who aren’t infected but are worried, they have the virus and are flooding healthcare facilities—are going through right now.
How hospitals can create a protective environment for nurses?
- Develop inpatient, ambulatory, and home care policies and procedures that are in line with current CDC guidelines for COVID-19.
- Provide training to all personnel on screening and isolation procedures.
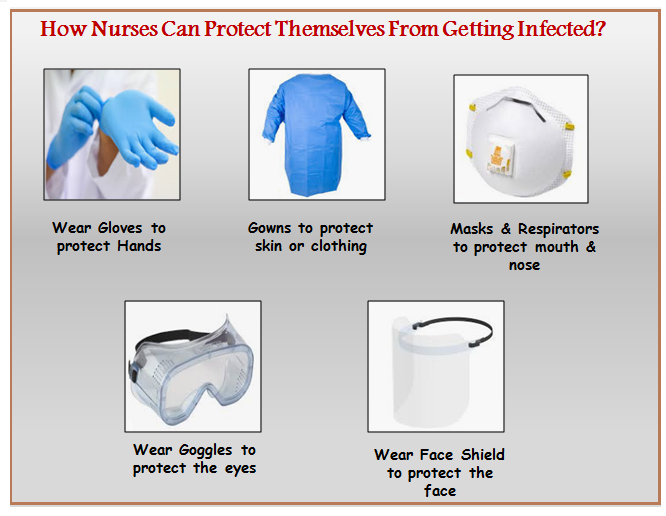
- Provide updated training and guidelines on the use of Personal Protective Equipment (PPE), such as the use of gloves, gowns, masks, eye protection, and a face shield.
- Clearly display signage for patients that list symptoms and instructions to wear a face mask before entering the healthcare facility if symptoms are present.
- Incorporate assessment questions to document a detailed travel history when patients present with fever, cough, or respiratory illness.
- Identify, in advance, airborne infection isolation rooms (AIIR) or negative pressure rooms, for quarantine and screening.
- Outline staffing protocols to facilitate the care of patients with COVID-19 and to minimize patient-to-patient and patient to staff transmission.
- Have available for immediate notification of suspected cases the infection control personnel at your facility and the local and state health department.
How the United States is preparing?
As the ICN outlined, one of the biggest threats that the U.S. will face if the coronavirus spreads as quickly as it did in China is a lack of personal protective equipment (PPE).
In an article for NPR, veteran nurse Maureen Dugan, who works at the University of California, San Francisco Medical Center, which treated two coronavirus patients this month, described how the Ebola crisis revealed how poorly prepared the healthcare community, in general, is to ensure the safety of healthcare workers.
She pointed out how the gowns they gave in the face of the Ebola crisis did not protect workers’ necks. “The gowns that they’re providing are inadequate,” she told NPR. “I’m sorry — I get very passionate about this because we’ve worked so hard to make sure that our nurses were protected and therefore, they can protect the patients.”
Unfortunately, most U.S. hospitals still are not adequately prepared with PPE, and a survey from the National Nurses United found that only 9% of hospitals had a specific plan on how to isolate infected patients, which is a grave situation and matter of concern. However, the White House has requested funding to prepare for the virus, so the hope is that hospitals and healthcare facilities will be more equipped to handle an incoming threat in the weeks and months ahead.
How nurses can stay protected?
Currently, the CDC explains that there is no vaccine or treatment for the virus; care is limited to supportive measures only. The organization is not recommending any sort of universal screening at this time yet. The CDC says that the exact way the virus is transmitted hasn’t been completely confirmed just yet, but coronavirus, in general, is transmitted through the air (think droplets, sneezing, coughing, etc.), which is why it is so highly contagious.
As of right now, there is no real reason to do anything other than standard precautions when caring for your patients, as with any suspected case of a respiratory virus (like the flu!). These include:
- Ensure the hospital’s protocol of using face masks for patients who you suspect are infected is followed.
- Above all, proper handwashing is always the most important step you can take.
- In the event that you do have a patient that meets the criteria for known or suspected 2019-nCoV, the CDC says that standard, contact, and airborne precautions should be used by all healthcare workers, and the patient should be placed into an AIIR immediately or transferred to a facility with an AIIR. In the event that neither of those things is available, they recommend isolating the patient as much as possible in a room where the air is not re-circulated without HEPA filtration and placing a surgical face mask on them.
Above all and re-stressing, the CDC is reminding everyone—nurses, healthcare workers, and the public alike—that the most important thing anyone can do to stop the spread of the virus and protect themselves is to continue to practice proper handwashing techniques, including using soap and water and scrubbing for at least one minute.
In the following video, a registered nurse talks about Coronavirus COVID-19 symptoms, causes, and prevention
How the novel coronavirus is spreading?
There’s still a lot we don’t know about how coronavirus spreads, according to the CDC. “Current knowledge is largely based on what is known about similar coronaviruses,” it said. “Most often, spread from person-to-person happens among close contacts (about 6 feet). Person-to-person spread is thought to occur mainly via respiratory droplets produced when an infected person coughs or sneezes, similar to how influenza and other respiratory pathogens spread. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. It’s currently unclear if a person can get 2019-nCoV by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes. There is much more to learn about the transmissibility, severity, and other features associated with 2019-nCoV, and investigations are ongoing.”
As for how coronavirus could pass from patients to nurses, that would most likely be via close contact, according to the CDC. This could include “being within approximately 6 feet (2 meters) of a patient with 2019-nCoV for a prolonged period of time” or “having direct contact with infectious secretions from a patient with 2019-nCoV. Infectious secretions may include sputum, serum, blood, and respiratory droplets. If close contact occurs while not wearing all recommended PPE, healthcare personnel may be at risk of infection.”
Who has novel coronavirus affected?
The deaths in China have seemed to be most prominent in susceptible individuals, similar to the flu, as it’s been reported that a 9-month-old infant and an 88-year-old man were both victims of the virus. And coronaviruses, in general, are associated with having higher mortality rates than the flu, so a lot remains yet to be seen to how the virus could affect the public.
According to the CDC, there are actually seven different types of coronaviruses that can currently infect humans, as well as three identified types that infect animals (but of course, those can jump to humans, as history has taught us). The type that is currently causing the outbreak in China is a brand-new virus from that has been named the 2019 Novel Coronavirus, or 2019-nCoV, for short, and it is in the same family as the SARs virus.
2019-nCoV has been described as a cross between the SARs virus and the MERs virus (both also coronaviruses), because it produces a very high inflammatory response in humans and infects both the upper and lower respiratory systems.
The 2019-nCoV is thought to have originated specifically from the wild animal market in Wuhan, which sells seafood, processed meats, and live animals and a new study has theorized the virus most likely came from snakes and somehow made the jump into infecting humans.
How dangerous is coronavirus?
The exact threat of the coronavirus is largely known to those of us in the U.S. right now. To put things into perspective, the CDC estimates that the influenza virus has already killed a significant amount of population globally and which some are saying is the most destructive one since the last World War II, so the growing number of cases of this brand-new virus in the country is definitely a matter of concern and emphasizes heavily on PPE – so our healthcare systems can help us win the battle against coronavirus and the need for personal hygiene in addition to social distancing.
To know more on the statistics of Coronovirus please click Coronavirus Disease (COVID-19) – Statistics and Research
“Hardships often prepare people for an extraordinary destiny.” —C.S. Lewis